Buying an air purifier for hospitals
Hospitals are places where people come for treatment and recovery. As such, these institutions should be safe havens for health and cleanliness. Unfortunately, this is not always the case. Hospital-inquired infections (HAIs), also known as ‘nosocomial infections’, are rising by 0.06% per year on a global scale1. These are infections contracted by patients whilst in a hospital setting. Many of these infections are spread via airborne viruses, emphasising the societal need of addressing the topic of poor indoor air quality (IAQ) in hospitals. How does a hospital’s indoor air quality (IAQ) impact patient well-being? Can an air purifier for hospitals help to reduce the number of pathogens spread by patients and particle pollution? Read on to learn more.

Major causes of poor air quality inside hospitals
Hospitals and other healthcare facilities suffer from two main types of indoor air pollution: chemical and biological. Since these institutions operate on a full-time basis, there is a constant influx of indoor air pollution that never has the opportunity to dissipate.
Chemical pollution
In hospitals, the use of sterilising, disinfecting, and cleaning products releases a host of volatile organic compounds (VOCs) that have negative health risks. Some of these may include gases and particles like formaldehyde and benzene (two known carcinogens), ethylene oxides, alcohols, carbon monoxide and dioxide, radon, and glutaraldehyde2,3. Furthermore, gases like nitrous oxide that are used for anaesthetic purposes and other medical procedures contribute to poor indoor air quality.
Studies have established that analysing and monitoring chemical pollution in hospitals are often given less attention than biological pollution. Concentration of VOCs in indoor spaces is often 2 to 5 times higher than outdoor spaces, sometimes reaching up to 1000 times higher just after using a product that emits VOCs4. Exposure to VOCs and particle pollutants can lead to both short-term and long-term health risks ranging from:
- Short-term: headaches, dizziness, eye and throat irritation, loss of coordination
- Long-term: nervous system, liver, and/or kidney damage; formaldehyde and benzene are carcinogenic3
Additionally, it is common for hospital buildings themselves to emit harmful air pollutants, causing occupants to experience Sick Building Syndrome. In order to emphasise energy efficiency, newer buildings have an airtight design. Once pollutants enter, they cannot escape, causing a build-up in pollutant concentrations. Materials used in construction like paints, solvents, adhesives, and even new furniture and other furnishings all release dangerous pollutants like VOCs (especially formaldehyde) into the interior of a building for up to two years!
Older hospital buildings have their own set of problems with contributing to poor indoor air quality. Outdated ductwork may mean improper filtration of air that is drawn in from outside. Chemical pollutants like VOCs and other types of air pollutants like dust and dust mites, dirt, pollen, and even airborne pathogens are able to circulate through vents, gaining access to vulnerable patients and staff.
The benefits of Eoleaf air purifiers for hospitals
-
Quiet yet powerful devices (up to 670 m3/hr)
-
Discreet and elegant design
-
Easy to use (equipped with Automatic mode) and does not require installation or assembly
-
Can be placed anywhere in your space thanks to our 360° technology
-
Real-time air quality data
-
Filters 99.97% of pollutants using unique and innovative filtration technologies
-
Can be controlled remotely via smartphone app
-
Smart and customisable devices (smart scheduling, automatic power off/on, etc.)
-
Mode automatique, mode silencieux et mode boost
Biological pollution
Naturally, biological pollution is the type of indoor pollution most commonly associated with a hospital environment. Based on systematic review on 55 hospitals in 14 different countries around the world, the World Health Organization (WHO) reports that 8.7% of patients receiving treatment in hospital had HAIs. Prevalence of HAIs was estimated at 5% in Europe and North America but was highest (upwards of 40%) in some African, Latin American, and Asian countries1.
When a patient coughs or sneezes, aerosols may be released into the air or spread onto hospital surfaces. These aerosols may land on materials like bedpans, silverware, bedding, and furniture. Coughing and sneezing may propel aerosols up to 60 metres (200 feet)9! This makes it easy for bacteria and viruses to circulate throughout the rest of the hospital, potentially infecting other patients and staff. The most common HAIs are respiratory tract infections (pneumonia), surgical site infections, sepsis, Clostridium difficile infections (CDIs), and urinary tract infections5.
HAIs and biological pollution can be spread in multiple ways:
- Poor hospital IAQ that spreads airborne pathogens
- Poor personal hygiene of hospital staff
- Poor hospital health standards
- Lack of compliance to established hospital health and safety guidelines6
With the proliferation of the SARS-CoV-2 virus during the COVID-19 pandemic, the importance of combatting airborne illness in hospitals has been put in the limelight. One study goes as far as to claim that ‘reasonable air quality control in hospital facilities is not only vital for infection prevention considering patients with weakened immune systems, it is also central toward ensuring healthcare workers' optimal health, productivity and well-being’7,8.

Poor ventilation
Hospitals and healthcare facilities are generally fragile environments. The goal is to keep vulnerable patients safe by keeping out outside contaminants wherever possible. With closed environments often comes lack of sufficient ventilation which causes severe problems for a hospital’s indoor air quality. Ventilation is crucial in controlling levels of indoor air pollution. It can even reduce pathogen transmission risk between patient rooms and within NHS institutions.
Coronavirus transmission in hospitals and the COVID-19 pandemic as a whole have put things into perspective. They have proven that greater attention must be paid by hospitals and other medical institutions in ensuring proper ventilation and maintenance of ventilation systems. This may include installing more specialised ventilation systems designed for healthcare buildings, an option that is usually costly but necessary for NHS institutions. When used in combination with medical-grade air purifiers installed in patient rooms and other high-transmission locations around a hospital, bacterial and viral transmission may be significantly reduced.
Outdoor factors contributing to poor hospital IAQ
Certain outdoor factors may contribute to poor air quality in a hospital environment. Firstly, levels of outdoor air pollution play an important role in indoor air pollution concentrations. Hospitals and healthcare facilities located in urban or industrial environments are impacted most by outdoor air pollution. In these areas, high levels of vehicle exhaust, pollution from construction sites, power plants, and smog are all sources of fine particle pollution (particulate matter). Patients may track particles from outdoors into hospitals on their clothes, on their skin, and in their hair. These fine particles may also enter hospitals via HVAC systems.
Rural environments equally have their share of particle contributions to poor indoor air quality in hospitals. Rural environments experience high levels of allergens, like pollen and road dust, and pesticides used on nearby agricultural lands.
Climate conditions like humidity and temperature may further aggravate poor indoor air quality in both urban and rural locations.
Occupational factors
Certain hospital-specific pollutants may pose dangers to NHS staff and patients alike. Mercury is one of those pollutants.
When a device containing mercury is broken, if proper measures are not taken to handle or store the broken device, mercury will be emitted into the indoor air. Without sufficient ventilation, toxic vapours may contaminate a hospital’s breathing air. Once mercury gains access to the body via inhalation, it can make its way to the bloodstream.
Mercury is a neurotoxin, and health risks depend upon many different factors including:
- The dose and type of mercury to which the person was exposed
- The age of the person
- The duration of exposure
- The route of exposure (inhalation, dermal, ingestion)
When mercury is airborne, inhalation can lead to negative effects on the nervous, immune, and systems as well as damage to the liver and kidneys. Behavioural and neurological effects are commonly observed, and foetuses are the most at-risk10.
Furthermore, staff members who are responsible for cleaning may experience high levels of exposure to VOCs, endangering their health. The presence of cleaning products in patient rooms may also impact the health of patients.

How does an air purifier for hospitals work?
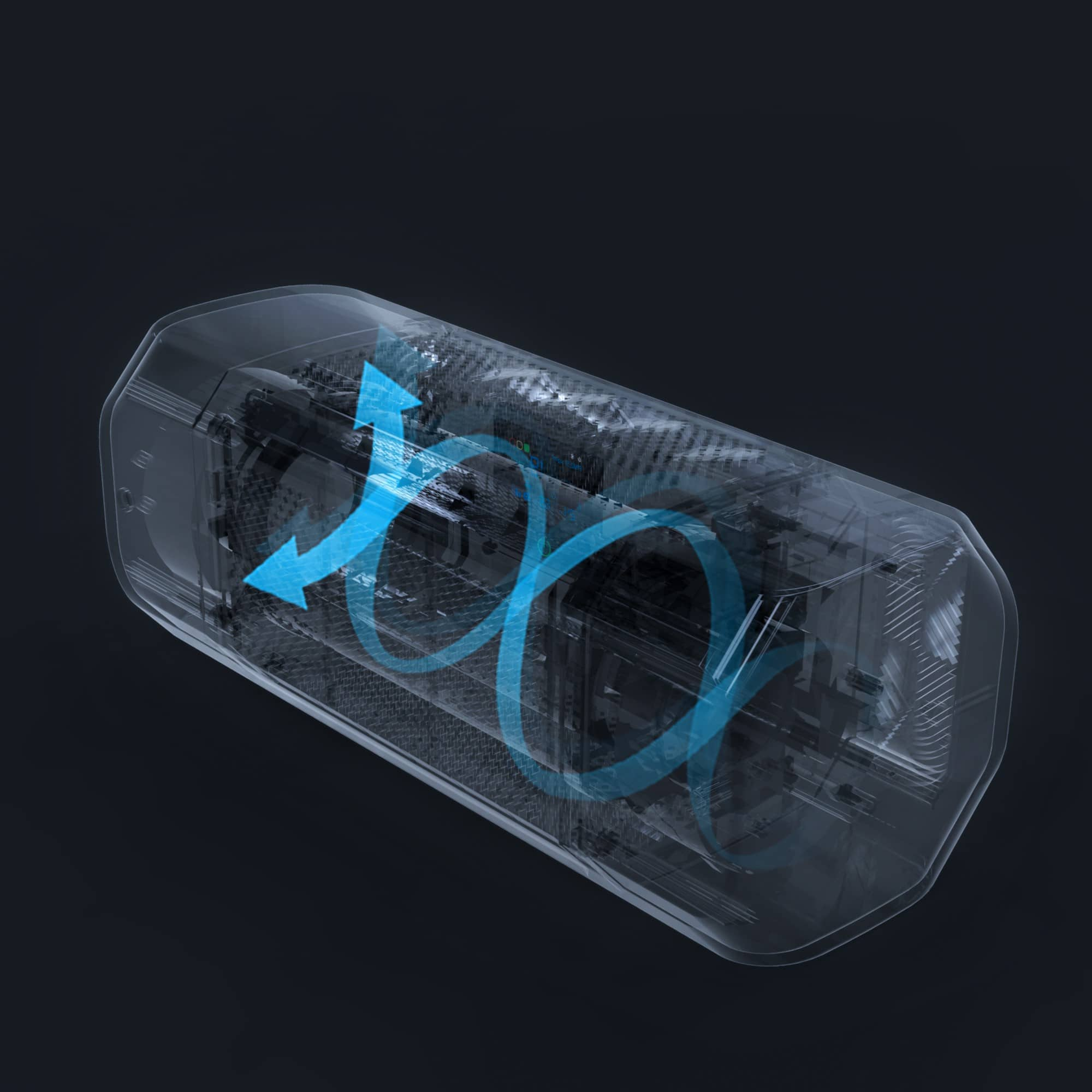
Air purifiers, also known as ‘air sterilisers’ or ‘air cleaners’, are powerful yet simple machines. They pull in polluted air containing toxic gases and particles from your indoor space, treat the air using one or more air filtration technologies, then release the purified air back into your space.
Air cleaners available on today’s market vary greatly in the options they offer and their price. Some are designed to combat specific types of pollutants, whereas others have a wider spectrum of action.
The benefits of an air purifier for hospitals
Installing air purifiers and investing in better IAQ in a hospital is a great way to protect recovering patients and hard-working staff.
Prevent an outbreak
As a result of the COVID-19 pandemic, the use of air purifiers in hospitals has risen significantly. Multiple studies have thus focused their efforts on understanding to which degree these devices help reduce pathogen transmission. As we have learned from the coronavirus pandemic, airborne pathogens like COVID-19 are transmitted through aerosol droplets and microdroplets. Exposure to these bacteria and viruses in hospitals or patient rooms occurs when an infected individual talks, coughs, sneezes, sings, or even breathes or exhales with their mouth open. Social distancing can sometimes pose challenges in hospitals when doctors need to be close to their patients. Pathogen transmission rates are highest in indoor spaces without proper ventilation that are occupied by many people, making a hospital the perfect breeding ground.
A 2023 study found that the correct use of a portable air cleaner (PAC) can reduce the half-lives of aerosols by 82%, thus serving as an excellent form of infection control. Furthermore, the study found that concentration levels of aerosols were at least 46% lower than environments without air cleaners. A portable air purifier can lead to ‘significant reductions in the level of aerosol concentration’, consequently reducing droplet-based airborne diseases and pathogens11.
Another 2021 study had even more promising results. It found that the use of two portable air cleaners in a single patient room found that within 5.5 minutes, 99% of aerosols were removed from the air12.
It is important to note that air sterilisers should not be used as a replacement for sufficient ventilation. In order to continue to support improved indoor air quality (IAQ) and infection control in a hospital, a combination of an air purifier for hospital use and ventilation is always recommended.
Reassure staff and patients
Studies have even shown that when patients know they are breathing cleaner air, it may aid in their recovery. A ‘healthy psychology’ and a reduction in stress can encourage earlier surgery recovery, improve the short- and long-term outcomes of chronic diseases and infections13.
The same can be said for members of hospital staff. When staff members feel that their employer is investing in their health by installing air purifiers in a hospital, they will feel empowered to put in more quality work. Furthermore, studies have linked the presence of indoor air pollution in the workplace with decreased concentration and productivity and increased fatigue. By improving indoor air quality in a hospital, staff may benefit from a 25% increase in productivity14.

Reduce hospital spending
A 2012 study out of California found that patients and staff are not the only ones to benefit from the installation of air purification devices in hospitals and other healthcare facilities. In fact, by focusing efforts on improving overall air quality, a hospital can significantly reduce its spending on air pollution-related equipment and patient care.
The economic costs of air pollution-related illness, especially emergency care for patients with asthma and respiratory and cardiovascular diseases, have grown dramatically in the past several decades. One hospital that took part in the study, Riverside Community Hospital in California, found that had federal standards been met for indoor and outdoor PM2.5 levels from 2005 to 2007, 329 air pollution-related hospital admissions and ER visits could have been prevented. These hospital admissions and ER visits equated to a total of over $2 million (£1.6 million or €1.8 million). Another hospital, St. Agnes Medical Center, had similar findings during this timeframe with 384 air pollution-related hospital admissions/ER visits totalling nearly $3 million (£2.3 million or €2.7 million)15.
Knowing that our indoor spaces are 2 to 5 times more polluted than outdoor spaces, investing in improved indoor air quality in hospitals can lead to noteworthy savings.
How to choose an air purifier for hospitals?
NeoPur 400 air purifier
40 m² (450 sq ft) coverage area - Smart & Connected
TeraPur 600 air purifier
80 m² (850 sq ft) coverage area - Ultimate all-in-one
AltaPur 700 air purifier
120 m² (1300 sq ft) coverage area - Professional model
Not all air cleaners offer the same technologies and options, nor are they all adapted to the versatile needs of a hospital. It is crucial to keep certain things in mind when shopping for the perfect device.
Consider the type and size of the room
A hospital has many different rooms and spaces, meaning that it has many different requirements when it comes to air purification. It may have patient rooms, waiting rooms, positive and negative pressure rooms, laboratories, transport units, emergency rooms, burn units, elderly care, ICUs, custodial spaces, and more. For a large space with so many needs, the best option is to choose an air purification device that can do it all.
A device that is portable, combats all types of pollutants, and with powerful airflow will enable you to place it wherever in your hospital, whenever. One crucial aspect to consider before making your purchase is to ensure that the air cleaner is properly sized to the volume of the room for which the device is intended! Air purifiers for hospitals are built to purify the air of a room of a maximum size. For large rooms and spaces, our AltaPur 700 air purifier would be ideal; for smaller rooms and spaces, our NeoPur 400 air purifier would be best.
Consider filter type and budget
As mentioned above, air purifiers for hospitals may come with many different types of technologies, meaning that average prices may range from £200 to £1000. The most common technologies you may find in an air steriliser are:
- Pre-filters
- Bamboo filters
- Lysozyme and silver ions
- Medical-grade HEPA-certified filters
- Note: you may come across ‘HEPA-type’ filters for certain air purification devices. Although cheaper, ‘HEPA-type’ filters do not undergo the same third-party testing undergone by HEPA-certified filters. As a result, they cannot be guaranteed the same level of filtration as HEPA-certified filters!
- Activated carbon filters
- Photocatalysis
- Ultraviolet (UVC) sterilisation
- Ionisation (negative ions)
When searching for an air purifiers for hospitals, it is particularly important to seek out a device containing a medical-grade HEPA-certified filter and UVC sterilisation at minimum. Although these technologies are extremely effective against fine particles and pathogens, they do not fight against chemical pollution like VOCs. In addition to HEPA-certified filtration and UVC sterilisation, Eoleaf’s air purifiers also come equipped with activated carbon and photocatalysis to fight against VOCs. A device like this enables you to combat all types of indoor air pollution in a hospital!
Additionally, your device’s filters should be easy to replace. Low-quality filters often require replacements multiple times a year, significantly contributing to the maintenance budget of your device. High-quality filters like Eoleaf’s only require replacement once a year. Furthermore, despite offering 8 different filtration technologies, our filters are all-in-one, making filter changes easy and feasible by anyone in just minutes.
Keep in mind that energy consumption also contributes to your budget. Choose an air purifier for a hospital that is energy-efficient, making for an eco-friendly and economical user experience. Lastly, not only should your air purifier for your hospital be durable, but the manufacturer should offer replacement parts and a dedicated repair centre to ensure long-lasting use. Eoleaf has two dedicated repair centres to ensure long-lasting use of your air cleaner, one in the UK and one in France.
Consider its noise level
An air purifier installed in a hospital should never be loud enough to disturb resting patients or medical staff performing their duties. Air sterilisers should never exceed 70 decibels (dB), keeping its fan noise low even whilst running on its top fan speed. A quiet device offering multiple fan speed levels is ideal as it adapts to the room it is in.
For assistance on our products or for sizing your project, do not hesitate to reach out to our team of air purification experts. Also feel free to refer to our Buying Guide for more information on how to choose an air purifier for your hospital.

Resources
1 Raoofi S, Pashazadeh Kan F, Rafiei S, Hosseinipalangi Z, Noorani Mejareh Z, Khani S, Abdollahi B, Seyghalani Talab F, Sanaei M, Zarabi F, Dolati Y, Ahmadi N, Raoofi N, Sarhadi Y, Masoumi M, Sadat Hosseini B, Vali N, Gholamali N, Asadi S, Ahmadi S, Ahmadi B, Beiramy Chomalu Z, Asadollahi E, Rajabi M, Gharagozloo D, Nejatifar Z, Soheylirad R, Jalali S, Aghajani F, Navidriahy M, Deylami S, Nasiri M, Zareei M, Golmohammadi Z, Shabani H, Torabi F, Shabaninejad H, Nemati A, Amerzadeh M, Aryankhesal A, Ghashghaee A. Global prevalence of nosocomial infection: A systematic review and meta-analysis. PLoS One. 2023 Jan 27;18(1):e0274248. doi: 10.1371/journal.pone.0274248. PMID: 36706112; PMCID: PMC9882897.
2 Fonseca, A.; Abreu, I.; Guerreiro, M.J.; Barros, N. Indoor Air Quality in Healthcare Units—A Systematic Literature Review Focusing Recent Research. Sustainability 2022, 14, 967. https://www.mdpi.com/2071-1050/14/2/967
3 El-Sharkawy MF, Noweir ME. Indoor air quality levels in a University Hospital in the Eastern Province of Saudi Arabia. J Family Community Med. 2014 Jan;21(1):39-47. doi: 10.4103/2230-8229.128778. PMID: 24696632; PMCID: PMC3966095.
4 Volatile organic compounds’ impact on indoor air quality. Environmental Protection Agency. (2023, August 15). https://www.epa.gov/indoor-air-quality-iaq/volatile-organic-compounds-impact-indoor-air-quality
5 Abdullah, M. (2021, January 28). 5 most common hospital acquired infections (HAIS). Inivos. https://inivos.com/blog/5-most-common-hospital-acquired-infections-hais/
6 Gozel MG, Hekimoglu CH, Gozel EY, Batir E, McLaws ML, Mese EA. National Infection Control Program in Turkey: The healthcare associated infection rate experiences over 10 years. Am J Infect Control. 2021 Jul;49(7):885-892. doi: 10.1016/j.ajic.2020.12.013. Epub 2020 Dec 25. PMID: 33359550.
7 Ibrahim F, Samsudin EZ, Ishak AR, Sathasivam J. Hospital indoor air quality and its relationships with building design, building operation, and occupant-related factors: A mini-review. Front Public Health. 2022 Nov 8;10:1067764. doi: 10.3389/fpubh.2022.1067764. PMID: 36424957; PMCID: PMC9679624.
8 Śmiełowska M, Marć M, Zabiegała B. Indoor air quality in public utility environments-a review. Environ Sci Pollut Res Int. 2017 Apr;24(12):11166-11176. doi: 10.1007/s11356-017-8567-7. Epub 2017 Feb 24. PMID: 28236201; PMCID: PMC5393278.
9 Air, Q. (2023). Hospitals & Healthcare. Hospital and Healthcare Air Quality and Solutions. https://quatroair.com/industries/hospitals-and-healthcare
10 World Health Organization. (2017, March 31). Mercury and Health. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/mercury-and-health
11 Salmonsmith J, Ducci A, Balachandran R, Guo L, Torii R, Houlihan C, Epstein R, Rubin J, Tiwari MK, Lovat LB. Use of portable air purifiers to reduce aerosols in hospital settings and cut down the clinical backlog. Epidemiol Infect. 2023 Jan 18;151:e21. doi: 10.1017/S0950268823000092. PMID: 36650731; PMCID: PMC9990385.
12 Buising KL, Schofield R, Irving L, Keywood M, Stevens A, Keogh N, Skidmore G, Wadlow I, Kevin K, Rismanchi B, Wheeler AJ, Humphries RS, Kainer M, Monty J, McGain F, Marshall C. Use of portable air cleaners to reduce aerosol transmission on a hospital coronavirus disease 2019 (COVID-19) ward. Infect Control Hosp Epidemiol. 2022 Aug;43(8):987-992. doi: 10.1017/ice.2021.284. Epub 2021 Jun 24. PMID: 34266516; PMCID: PMC8314194.
13 Mavros MN, Athanasiou S, Gkegkes ID, Polyzos KA, Peppas G, Falagas ME. Do psychological variables affect early surgical recovery? PLoS One. 2011;6(5):e20306. doi: 10.1371/journal.pone.0020306. Epub 2011 May 25. PMID: 21633506; PMCID: PMC3102096.
14 Neidell, M., Pestel, N. Air pollution and worker productivity. IZA World of Labor 2023: 363. doi: 10.15185/izawol.363.v2
15 Romley, J. A., Hacksbarth, A., & Goldman, D. P. (2012). The Impact of Air Quality on Hospital Spending. RAND Corporation. https://www.rand.org/pubs/periodicals/health-quarterly/issues/v2/n3/06.html
Eoleaf's range of air purifiers
NeoPur 400 air purifier
40 m² (450 sq ft) coverage area - Smart & Connected
TeraPur 600 air purifier
80 m² (850 sq ft) coverage area - Ultimate all-in-one
AltaPur 700 air purifier
120 m² (1300 sq ft) coverage area - Professional model
PurCar air purifier
HEPA H13 Filter & Ioniser - For all vehicles